Symptoms of Retinal Disease
Floaters
Floaters arise from the gel structure that fills the center of the eye, known as vitreous. At birth and during youth, the vitreous is a solid, clear gel.
Eye Before Floater Vitrectomy

Eye After Floater Vitrectomy
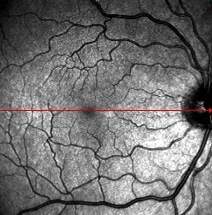
During aging, the gel turns to liquid with strands of aggregated collagen. When the gel vitreous is highly liquefied, it can no longer fill the center of the eye and it collapses, pulling away from the retina. This causes the sensation of dark, linear, hair-like or fly-like images that move with eye movement, causing a floating sensation. Floaters are sudden and most noticeable in bright light situations, especially when looking at the sky or a bright white surface. Floaters can sometimes be bothersome enough to be very troubling to patients, as recently proven by a study in a Singapore and pointed out by Dr. Sebag in a publication in the American Journal of Ophthalmology. Floaters can be treated by Dr. Sebag.
Read how this treatment worked for others.
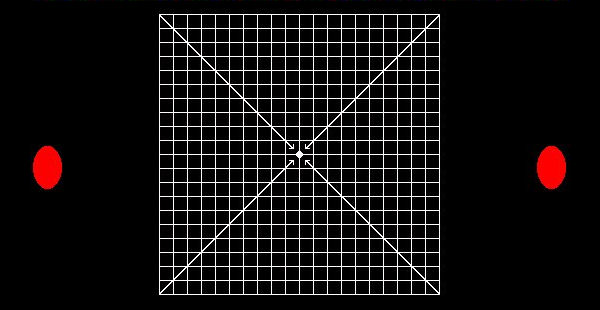
Distortions
Distortions could indicate a problem in the Macula, the center of the retina. If you close one eye and look at something that should be straight, like the edge of a door, blinds on a window, or the grid shown below, you should not see distortions.
The sudden onset of distortions in an elderly person could be due to Macular Degeneration. In a middle-aged person, the sudden onset of distortions could be the results of a Macular Hole or fluid in the macula from various sources, including diabetic retinopathy. Distortions should be evaluated at the VMR Institute, where new tests are being developed in conjunction with the Jet Propulsion Laboratory, Caltech, and The Doheny Eye Institute which will detect distortions sooner and more accurately. This will enable prompt therapy at the VMR Institute, which is always more effective.
Flashing Lights
If vitreous pulls on the retina while it pulls away, it can rip the retina. If you experience flashing lights that are linear (not speck-like), arc-shaped, and situated off to the side, you are at risk of a retinal tear, especially if the flashing lights are triggered by turning the head or moving the eyes back and forth. Flashing lights should be evaluated immediately, since a torn retina can be repaired with an office procedure, avoiding the need for hospital surgery.
Dark Curtain
A torn retina can allow fluid to enter the space behind the retina and lift it off the back of the eye, called a Retinal Detachment. The result is the sudden onset of peripheral (off to the side) vision loss seen as a curtain or darkness with a curved demarcation line. On the inside of the line, vision is normal. On the outside of the line, everything is gray or dark. To preserve central vision, this must be promptly evaluated and treated.

